PERIODONTAL DISEASE
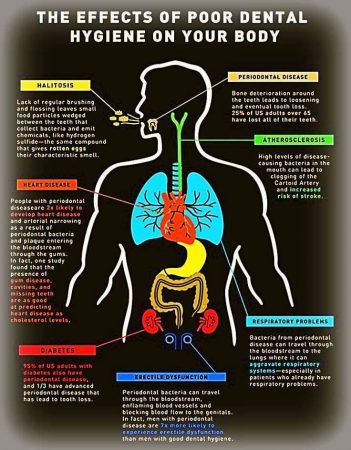
Periodontal disease is perhaps one of the most common afflictions shared by almost everyone. There are degrees and stages to the disease. Treatment is best done as a collaboration between your dentist and you. You MUST do your part if you wish to make any headway with this disease. If you don’t treat it you can very well lose bone, loose teeth, suffer bleeding gums and could very well end up without any teeth. It also does not just affect the mouth, your gums and teeth, but it can affect your heart, increasing risk of heart disease, increase risk of respiratory disease and worsen diabetes.
As in any disease three are progressive step in its evolution and depending on where you catch it, the solution is either easy or much more involved and possibly invasive.
Gum disease has different stages. The mildest form of periodontal disease is gingivitis. It causes the gums to become red, swollen and bleed easily, especially when brushing or flossing. You might notice some discoloration on your teeth. This is called plaque. Plaque is a buildup of bacteria and food debris on your teeth. Although bacteria are always present in your mouth, they only become harmful when conditions allow them to increase dramatically. This happens if you don’t brush or floss, or get hygiene cleanings on a regular basis. Untreated it can advance to periodontitis and can eventually lead to tooth loss and other health problems.

Factors that may contribute to gingivitis include, diabetes, smoking, aging, genetic predisposition, systemic diseases and conditions, stress, inadequate nutrition, puberty, hormonal fluctuations, pregnancy, substance abuse, HIV infection and certain medication use.
Gingivitis is often caused by inadequate oral hygiene. The wonderful thing is that gingivitis is reversible with professional treatment and good oral home care.
Untreated gingivitis can advance to periodontitis. With time, plaque can spread and grow below the gum line. Toxins produced by the bacteria in plaque irritate the gums. The toxins stimulate a chronic inflammatory response in which the body in essence turns on itself and the tissues and bone that support the teeth are broken down and destroyed. Gums separate from the teeth, forming pockets (spaces between the teeth and gums) that become infected. As the disease progresses, the pockets deepen and more gum tissue and bone are destroyed. Often, this destructive process has very mild symptoms. Eventually, teeth can be come loose and may have to be removed.
Periodontal disease refers to any disease that affect the areas around the teeth (from the Latin “peri” – around and Greek “odont” – tooth). Periodontists are dentistry’s experts in treating periodontal disease. They receive up to three additional years of specialized training in periodontal disease 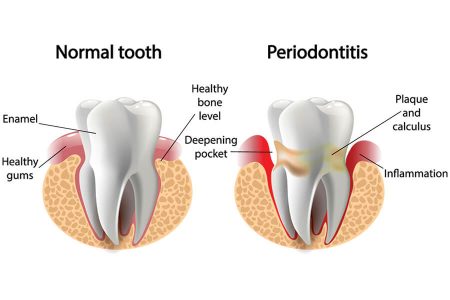 treatment in both non-surgical treatments and periodontal plastic surgery procedures. Periodontists are also experts in replacing missing teeth with dental implants.
treatment in both non-surgical treatments and periodontal plastic surgery procedures. Periodontists are also experts in replacing missing teeth with dental implants.
For the most part, periodontal disease is asymptomatic, especially in its early stages. The biggest symptom you’d usually see is the bleeding when brushing or flossing. By the time the major symptoms such as receding gums, pain when chewing, tooth loss, foul taste in your mouth, inflammatory response throughout your body, it is likely you’re advancing into the advanced stages of periodontitis.
The most effective treatment to halt or eradicate many forms of periodontal disease is preventative, performed by the patient. Good personal daily oral hygiene, which disrupts the growth of plaque, is the best defense.
Periodontal disease is the most prevalent disease in adults but the most untreated, at least until the later stages when the symptoms become more noticeable unless regular visits to the dentist are a part of that persons routine.
TREATMENT
As stated previously, good oral hygiene is the best preventative action one can take toward this disease. The main aim with any treatment for this is to clean out the bacteria from the pockets around  the teeth and prevent further destruction of bone and issue.
the teeth and prevent further destruction of bone and issue.
Proper dental care involves brushing teeth at least twice a day and flossing once per day. If there is enough space between the teeth, an interdental brush is recommended.
Soft-picks can be used when the space between the teeth is smaller. Patients with arthritis and others with dexterity issues may find that using an electric toothbrush is better for a thorough cleaning.
SCALING AND CLEANING
It is important to remove the plaque and calculus to restore periodontal health.
A healthcare professional will carry out scaling and debridement to clean below the gumline. This may be done using hand tools or an ultrasonic device that breaks up the plaque and calculus. Root planing is done to smooth rough areas on the roots of the teeth. Bacteria can lodge within the rough patches, increasing the risk of periodontal disease.
Depending upon how much plaque and calculus there is, this may take one or two visits.
Cleaning is normally recommended twice per year, and possibly more often, depending on how much plaque accumulates.
MEDICATIONS
There is currently no efficacious medication for this disease.
Oral antibiotics: Available in capsule or tablet form, these are taken orally. They are used short-term for the treatment of acute or locally persistent periodontal infection.
ADVANCED PERIODONTITIS
If good oral hygiene and non-surgical treatments are not effective, surgical intervention may be needed.
OPTIONS INCLUDE:
Flap surgery: The healthcare professional performs flap surgery to remove calculus in deep pockets, or to reduce the pocket so that keeping it clean is easier. The gums are lifted back, and the tarter is removed. The gums are then sutured back into place, so they fit closely to the tooth. After surgery, the gums will heal and fit tightly around the tooth. In some cases, the teeth may appear longer than before.
Bone and tissue grafts: This procedure helps regenerate bone or gum tissue that has been destroyed. New natural or synthetic bone is placed where the bone was lost, promoting bone growth.
Guided tissue regeneration (GTR) is a surgical procedure that uses barrier membranes to direct growth of new bone and gum tissue at sites where one or both of these are lacking. It aim to regenerate tissue and repair defects that have resulted from perio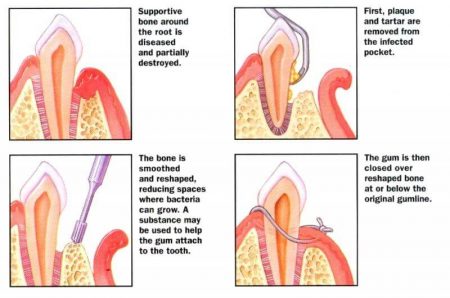 dontitis.
dontitis.
In this procedure, a small piece of mesh-like material is inserted between the gum tissue and bone. This stops the gum from growing into bone space, giving the bone and connective tissue a chance to regrow. The dentist may also use special proteins, or growth factors, that help the body regrow bone naturally.
The dental professional may suggest a soft tissue graft. This involves taking tissue from another part of the mouth, or using synthetic material to cover exposed tooth roots.
Success depends on how advanced the disease is, how well the patient adheres to a good oral hygiene program, and other factors, such as smoking status.
RISK FACTORS
Gum disease is more likely to become severe if there are high levels of aggressive bacteria, and if the person’s immune system is weakened.
 The following risk factors are linked to a higher risk of periodontitis:
The following risk factors are linked to a higher risk of periodontitis:
Smoking: Regular smokers are more likely to develop gum problems. Smoking also undermines the efficacy of treatment. Ninety percent of cases that do not respond to treatment are in smokers.
Hormonal changes in females: Hormonal changes occur during puberty, pregnancy, and menopause. These changes increase the risk of developing gum disease.
Diabetes: Those living with diabetes have a higher incidence of gum disease than other individuals of the same age.
AIDS: Gum disease is more common in people with AIDS.
Cancer: Cancer and some cancer treatments can increase the chance of gum disease.
Drugs: Medications such as antihypertensive drugs or vasodilating agents—which relax and dilate the blood vessels—immunotherapy drugs, and medications that reduce saliva can all increase the chance of gum disease.
Genetic factors: Some people are more susceptible to gum disease due to genetic factors.
DIAGNOSIS
A dentist can normally diagnose periodontitis by looking at the signs and symptoms and carrying out a physical examination.
The dentist will probably insert a periodontal probe next to the tooth, under the gum line. If the tooth is healthy, the probe should not slide far below the gum line. In cases of periodontitis, the probe will reach deeper under the gum line. The dentist will measure how far it reaches.
An X-ray may help assess the condition of the jaw bone and teeth.
COMPLICATIONS
The most common complication is the loss of teeth, but periodontitis may impact a person’s overall health in other ways.
It has been linked to a higher risk of a range of other diseases, including respiratory problems, stroke, and coronary artery disease, although how they are linked remains unclear.
One study of people with chronic coronary artery disease, lasting 3.7 years, found that for every five teeth lost, there was a 17-percent higher risk of cardiovascular death, a 16-percent higher risk of all-cause death, and a 14-percent higher risk of stroke.
Scientists are not yet certain why this happens. It may be that bacteria from periodontitis infects the coronary arteries, that the periodontal bacteria trigger an overall immune response that affects the cardiovascular system, or there may be another link.
It remains unclear whether gum disease leads to heart disease or the other way round. There is no evidence as yet that better oral care will lead to better cardiovascular health.
During pregnancy, if a bacterial infection causes moderate-to-severe periodontal disease, there is a higher risk of preterm birth. Periodontitis has also been linked to low birth weight and pre-eclampsia.
Postmenopausal women with periodontal disease are more likely to develop breast cancer, according to research published in Cancer Epidemiology, Biomarkers Prevention. Those with a history of smoking are particularly affected.
Periodontitis can also make it harder for patients with diabetes to control blood sugar.
See your dentist regularly and don’t let gingivitis progress through worse stages and suffer through all the complications. And brush your teeth twice a day!
Go Back